National Medical Health Card 26 Harbor Park Drive, Port Washington, NY 11050
Business Pharmacy benefits management
Key Business Executive Chairman James J. Big
Key Technology Executive CIO Agnes Hall
Project Establish database and analysis infrastructure to provide better service and anticipate growth.
Objective Provide faster answers to customer requests.
Technology Used Oracle on HP-UX, Oracle data warehouse tools
How it gave edge over bigger companies Gave NMHC customers direct access to data they needed to control their drug costs.
Last year, Beth Skalitzky dumped Medco Health Solutions, the $34 billion manager of pharmacy benefits for corporations. She felt she was operating in the dark. “We were not able to get our hands on data to help us manage our plan,” she says.
As benefits administrator for Perry Judds, a printing company based in Waterloo, Wis., she was frustrated that Medco wasn’t quicker to respond when she asked for reports on drug cost trends or explanations of problems reported by employees.
So Skalitzky switched to National Medical Health Card Systems (NMHC), a much smaller benefits manager that has annual sales of $651 million. A big part of the appeal: the ease with which she can get information from NMHC’s Web site.
More than 2,000 employees have her name and home phone number, and they weren’t afraid to use it when they had problems with Medco, such as getting to the prescription counter and not being given the proper discounts. “I remember one Fourth of July, I spent the whole day dealing with these sorts of problems,” Skalitzky says.
Now, her employees can find answers for themselves on NMHC’s site. Or, she can access their accounts and look things up quickly as well.
That NMHC was much smaller, with less than 2% of Medco’s sales, didn’t bother her. Medco serves more than 60 million “covered lives,” i.e., individuals and their dependents.
“As a 2,000-life company, we’re nothing to them,” Skalitzky says.
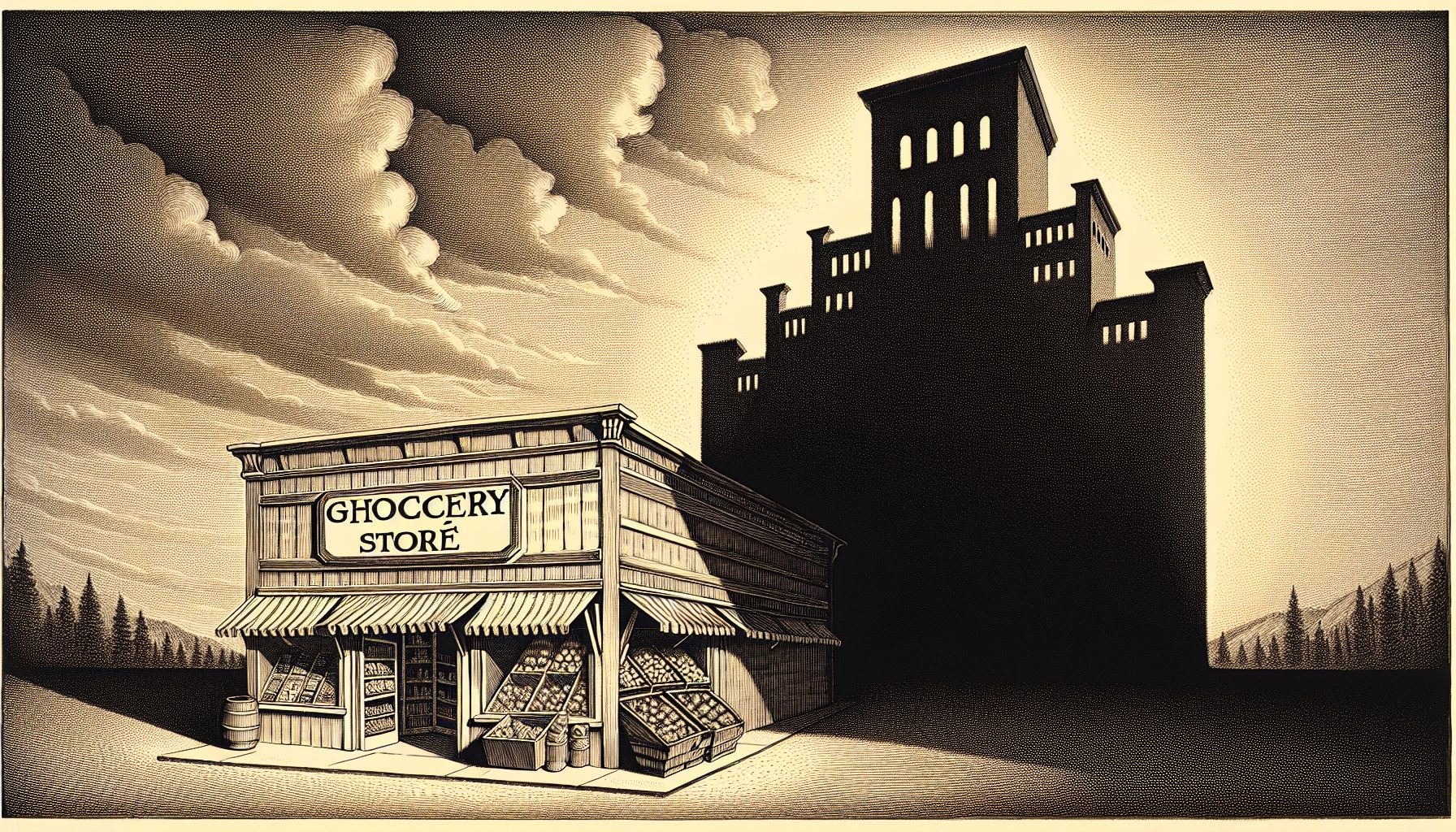
By contrast, it’s much easier to get NMHC’s attention. That’s why CIO Agnes Hall pushes to install systems that let NMHC respond quickly to customers.
Nobody’s going to get fired for picking Medco, Express Scripts or Caremark, but you will not get the personal care from those companies because they’re too big,” Hall says. “We want to offer very personal quality service that the big guys can’t offer, and to keep doing it no matter how big we get.”
How big is that?
For the past two years, NMHC has captured a spot in Fortune magazine’s list of the 100 fastest-growing companies in America. According to Fortune‘s September 2004 list, the company ranked sixth, with yearly growth of 44% and a 107% total return to investors over the past three years. NMHC was No. 27 on the list a year ago.