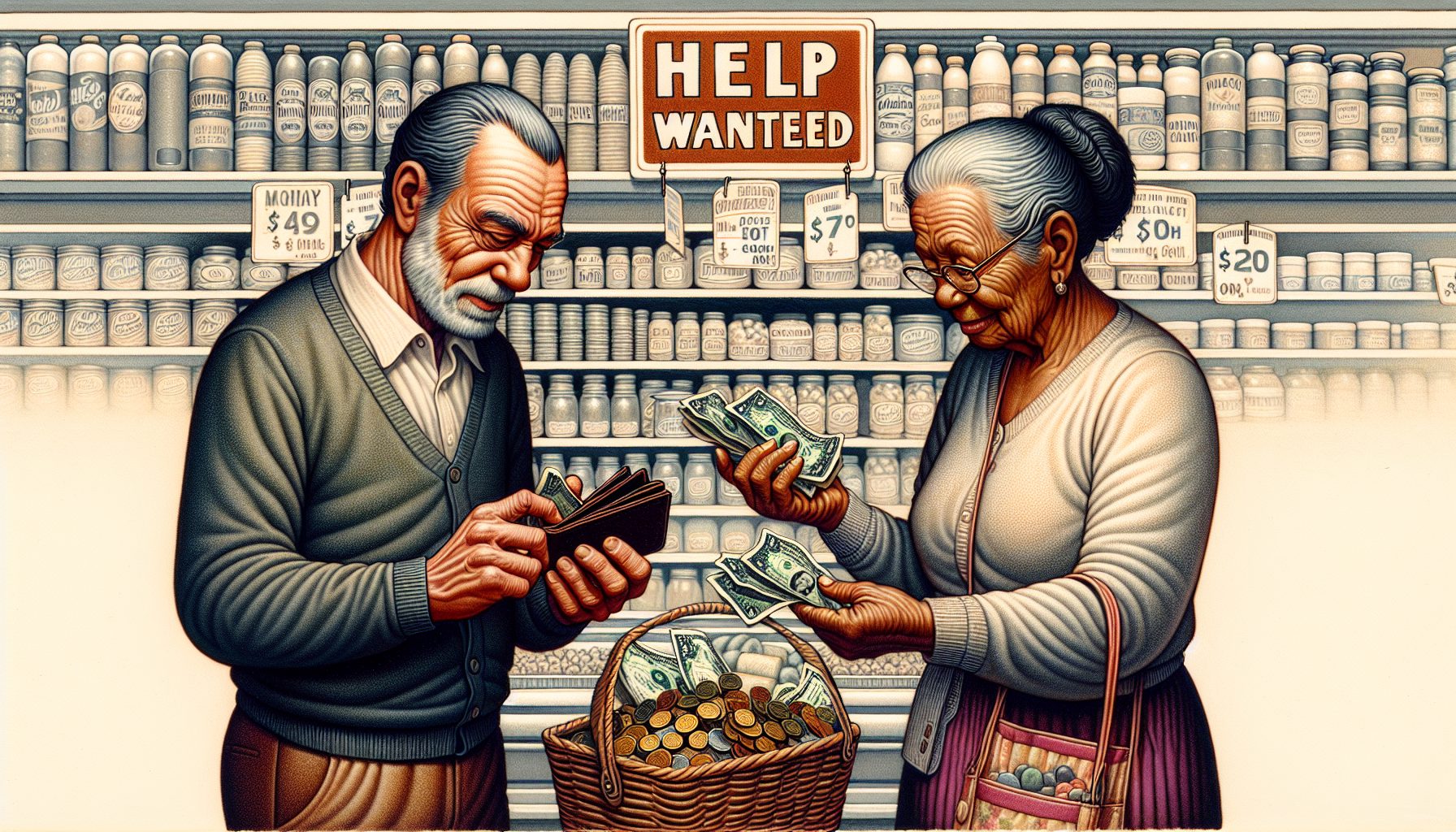
As the year ended, Bonnie Burns—a training and policy specialist with California Health Advocates, a nonprofit that counsels people on Medicare—was stretched to the limit.
She was swamped with requests for help from senior citizens afraid of losing coverage for their prescription drugs under the new Medicare drug benefit, which took effect on Jan. 1, 2006.
Her own stepfather was having problems, too. In November, she couldn’t figure out if the nine drugs he takes for a lung condition would be covered under his new plan.
Under the program, her stepfather and all other recipients of Medicaid—a joint federal-state program—who had been receiving their drug coverage from the states were automatically assigned to insurance companies that are supposed to be covering their drugs on behalf of the federal government.
But the Medicare Web siteand her parents’ insurance plan, SecureHorizons from PacifiCare, were giving Burns conflicting information.
Burns is not alone. Across the country, seniors and those caring for them remain uncertain as to what, if any, prescription drug coverage they’ll have under the new program.
On Dec. 22, 2005, the Department of Health and Human Services said 21 million people were enrolled in the plan. The program—under which, for the first time, the federal government will offer to subsidize prescription drug costs for everyone enrolled in Medicare, currently 43.1 million people—is complicated.
California, for example, offers 47 different statewide plans that cover drugs, plus 85 local plans that cover medications and other health care. Seniors and their advocates must sort through an array of choices from private insurers, whose plans differ in how much they charge, which drugs they cover and which pharmacies they allow seniors to use.
And the computers powering the program haven’t helped the situation. The system has run into a number of problems, which have ranged from Web site crashes that prevented people from signing up online, to the failure to match state and federal files of beneficiaries, to the inability to display online information for beneficiaries to review.
But Peter Ashkenaz, a spokesperson for the federal CMS (Centers for Medicare & Medicaid Services), said that “the systems we have are all working, and millions of people around the country are all getting their drugs.”
CMS would not say which systems handle which functions. And it’s unclear what systems are at the heart of the problems, or which problems are caused by applications installed for the new program as opposed to older ones that CMS has used to shuttle information between federal and state governments, pharmacies and insurance providers.
But new glitches persist. On Jan. 2, the database used by pharmacists to see whether people are eligible for coverage so they can dispense and bill for medication was overwhelmed with queries.
So many people showed up at pharmacies that day without evidence that they were enrolled in a health plan—either with a letter acknowledging that their application had been received or an enrollment card—that the pharmacists’ queries rendered the system at times unusable, according to federal contractor NDCHealth (now part of Per-Se Technologies), which administers the data repository.
In turn, pharmacists’ calls to insurers and CMS to verify the customers’ eligibility created backlogs on the phone lines.
Adding to the problem: As 2005 wound down, some people had switched plans, and the database didn’t always reflect the changes.
Enrollment files pass electronically from the health plans to CMS to NDCHealth. And, according to Robert Borchert, a spokesperson for NDCHealth, some of the data files that the contractor received from CMS were blank except for the name, which slowed processing time.
By Jan. 6, pharmacists said they were no longer having problems accessing the database, but the Minnesota Pharmacists Association says its members are still finding information that is missing or wrong. The database has also been providing incorrect co-payments for some beneficiaries in Minnesota and other states.
Next page: A $2.4B budget and an IT overhaul weren’t enough.